LOUISVILLE, Ky. (WDRB) -- Indiana's governor is trying to ease health care costs for Hoosiers.
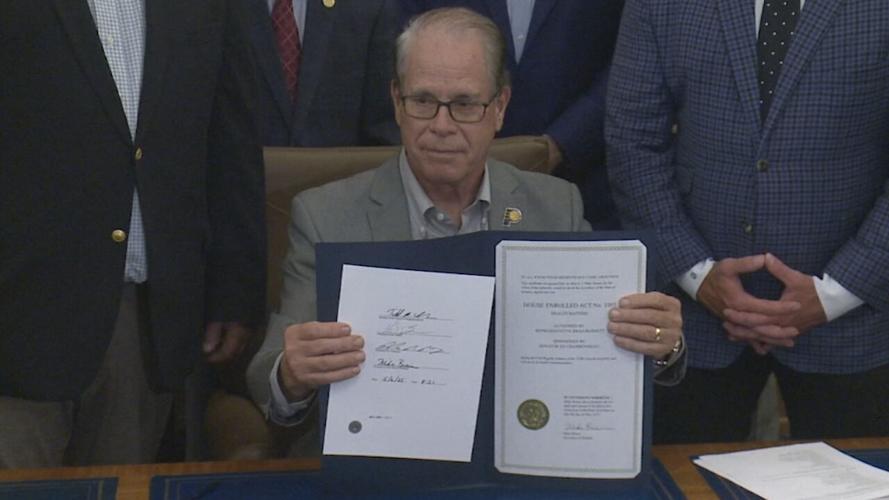
Gov. Mike Braun signed 10 health care-related bills he said will bring "substantial reform to health care" in the Hoosier state during a ceremonial bill signing Wednesday.
"These landmark bills bring transparency, accountability and competition to our health care system," Braun said.
The bills are designed to, in part, crack down on the rising costs of health care in Indiana, make the state a national leader in health care reform and price transparency, and eliminate "the anti-competitive practices and misaligned incentives that drive up hospital prices."
"I promised Hoosiers I would take on the big health care industry and get solutions to the problems making health care unaffordable," Braun said in a news release.
The governor said the bills "address systemic problems with the health care industry" by providing solutions. According to a news release from the governor's office, those include:
- Full hospital price transparency, requiring "good faith estimates" for health care services at least two days in advance, allowing patients to know what something costs upfront.
- Increasing market competition by ending "anticompetitive practices in physician non-compete agreements.
- Driving down prescription drug prices by reforming how pharmacy benefit managers operate.
- "Establishing that health plan administrators have a fiduciary duty to act in the best interest of the patients they act on behalf of."
- New accountability measures to ensure nonprofit hospitals "actually act like nonprofits."
One bill falls in line with the Braun's executive order adding new Medicaid work requirements and more eligibility checks.
Other bills prevent insurance companies from making patients pay more for certain medications than someone who uses a coupon and make health care ownership more transparent.
There is also a bill that helps Hoosiers with cancer by cutting red tape for organizations wanting to help cover the cost of clinical trials.
Bills signed, provided by Braun's office:
- House Enrolled Act 1003: "Patient-centric, landmark health care solutions package"
- Incorporates several provisions to bring transparency, accountability and enforcement mechanisms to the health care industry in the Hoosier state.
- Hospital cost transparency
- Requires a nonprofit hospital system to submit audited financial statements and provides for a $10,000 per day penalty for failure to submit the statements to the state
- Requires the office of management and budget to develop a methodology to be used in conducting a study of commercial inpatient hospital prices and outpatient hospital prices and to determine Indiana's statewide average inpatient and outpatient hospital prices
- By 2029, requires an Indiana nonprofit hospital system's aggregate average inpatient and outpatient hospital prices to at least be equal to or less than the statewide average.
- Established a Medicaid state directed payment program for hospitals
- Directed payments to be included in the managed care capitation rates (not separate payment term)
- Allows FSSA to designate provider classes in a way to incentivize hospitals to lower ACR and using data from the hospital audited financial statements submitted to the state
- Established a managed care assessment fee
- Allows for FSSA to submit a request for a tax waiver for the creation of the assessment fee
- The assessment fee may be used to fund the Medicaid program
- Revises disproportionate share (DSH) payments
- Pauses most DSH payments when a state directed payment program is in effect
- Allows FSSA to submit a SPA to develop and implement DSH payments for state
- Incorporates several provisions to bring transparency, accountability and enforcement mechanisms to the health care industry in the Hoosier state.
- HEA 1004: "Lowering hospital prices for Hoosier patients"
- Introduces a number of initiatives aimed at lowering hospital costs and addressing Medicaid financing and reimbursement.
- Senate Enrolled Act 2: "Making Medicaid more sustainable"
- Creates several Medicaid reforms around eligibility, reporting, work requirements and presumptive eligibility.
- SEA 3: "Fiduciary duty in health plan administration"
- Requires pharmacy benefit managers (PMBs) and third-party administrators (TPAs) to have a fiduciary duty to the plan sponsor that they are acting on behalf of.
- Allows FSSA to submit a SPA to develop and implement DSH payments for state
- Act with loyalty and care in the best interest of the plan sponsor;
- Ensure all fees, costs, and commissions are disclosed to the plan sponsor;
- Avoid self-dealing and conflicts of interest; and
- Maintain transparency in all financial and contractual arrangements related to the plan sponsor’s health insurance coverage, including prescription drug benefits.
- Requires pharmacy benefit managers (PMBs) and third-party administrators (TPAs) to have a fiduciary duty to the plan sponsor that they are acting on behalf of.
- SEA 140: "Reforming pharmacy benefit managers"
- "Prohibits PBMs from utilizing anti-competitive contracting and business practices against pharmacies, including retroactively denying, reducing reimbursement, or seeking refunds or recoupments for a dispensing claim paid to a pharmacy, penalizing a pharmacy for selling a lower cost alternative to an insurer, limiting or preventing a patient from obtaining medication from a non-affiliated pharmacy, including specialty drugs, discriminating against pharmacies located within the health plan’s geographic coverage area and is willing to participating in the health plan’s network, including all-or-nothing clauses in contracts with pharmacies to require additional contracting with affiliates of the insurer, PBM, or administrator, and reimbursing a pharmacy at a net amount that is either less than what the insurer or PBM would reimburse itself or an affiliated pharmacy for the same prescription drug by national drug code number or the national average drug acquisition cost (NADAC) plus a fair pharmacy dispensing fee."
- SEA 118: "340B Drug Program Report"
- "Requires covered entities participating in the 340B Discount Drug Program, as well as contract pharmacies and child sites, to annually report certain information and financial transactions to the Indiana Department of Health (IDOH). Failure to report the required information will result in the issuance of a civil monetary penalty of $1,000 per day."
- SEA 475: "Ending anti-competitive practices in physician noncompete agreements"
- "Prohibits hospitals, including a parent company or affiliated manager of a hospital and hospital systems, from requiring a physician to enter a noncompete agreement after July 1, 2025."
- HEA 1604: "Cost Sharing; Out-of-pocket expense credit"
- "Requires health plans to credit the amount paid for a lower cost, out-of-pocket health care service towards and individual’s deductible, regardless of whether the service was provided by an in-network or out-of-network provider. Additionally, insurers and health plan administrators are required to apply the annual cost sharing limitation prescribed under the Patient Protection and Affordable Care Act for prescription drugs that are covered under the health plan, are life-saving or intended to manage chronic pain, and do not have an approved generic equivalent."
- HEA 1666: "Ownership of health care providers"
- "Requires hospitals, insurers, PBMs, TPAs, and entities that accept Medicaid and Medicare to report ownership information to the State, and authorizes the Indiana Attorney General to investigate market concentration of a health care entity and review the ownership information submitted to the State."
- SEA 480: "Prior Authorization"
- This legislation revises Indiana’s prior authorization regulatory framework to better protect the provider-patient treatment plan and timely access to care.
For a list of House and Senate bills signed this legislative session in Indiana, click here.
Top Stories:
JCPS chooses million-dollar software to map out new bus routes
With no body or weapon, the circumstantial case against Brooks Houck begins Tuesday
Brooks Houck, Joseph Lawson moved to Bowling Green for Crystal Rogers murder trial
New Albany grocery store sells winning Powerball ticket worth $50,000
Copyright 2025 WDRB Media. All Rights Reserved.